News
CD4⁺ T cells help restore antiviral immunity in the liver by activating Kupffer cells to produce IL-27
Chronic hepatitis B virus (HBV) infection affects nearly 300 million people worldwide and is a major cause of liver disease, including cirrhosis and hepatocellular carcinoma. One of the key barriers to curing chronic HBV is the failure of the immune system—particularly CD8-positive (CD8⁺) T cells, which normally eliminate infected cells and suppress viral replication. In chronic infection, these cells become dysfunctional and unable to control the virus, prompting efforts to develop strategies that can restore their activity.
CD4-positive (CD4⁺) T cells are known to support immune responses, but whether and how they help CD8⁺ T cells during chronic hepatitis B have remained poorly understood. Now, researchers led by Professor Matteo Iannacone, Director of the Division of Immunology, Transplantation and Infectious Diseases at IRCCS Ospedale San Raffaele, Group Leader of the Dynamics of Immune Responses Lab, and Professor of Pathology at Vita-Salute San Raffaele University have discovered a previously unknown immune mechanism that takes place directly in the liver. Their findings have just been published in Nature Immunology.


The "Dynamics of Immune Response" Lab
The study
To explore the role of CD4⁺ T cells in liver immunity, the research team used an experimental system in mice, in which HBV replicates in liver cells, mimicking some features of chronic viral antigen exposure. Researchers introduced HBV-specific CD4⁺ and CD8⁺ T cells and observed if, where and how these cells interacted.
The presence of CD4⁺ T cells dramatically improved the ability of CD8⁺ T cells to expand, accumulate in the liver, and reduce viral replication. Crucially, this effect did not depend on traditional lymphoid organs such as the spleen or lymph nodes, suggesting that CD4⁺ T cells were delivering their support directly within the liver.
Using advanced microscopy, the researchers visualized direct interactions between CD4⁺ T cells, CD8⁺ T cells, and Kupffer cells, the specialized macrophages that line the liver’s blood vessels. They showed that CD4⁺ T cells “licensed” Kupffer cells through a molecular interaction known as CD40–CD40L, prompting the production of interleukin-27 (IL-27), a key immune messenger. When IL-27 production was blocked, CD8⁺ T cells remained dysfunctional—highlighting IL-27 as an essential mediator in this immune circuit.
Finally, the team demonstrated that administering IL-27 alone was sufficient to restore antiviral CD8⁺ T cell activity, both in mice and in immune cells isolated from patients with chronic HBV infection.
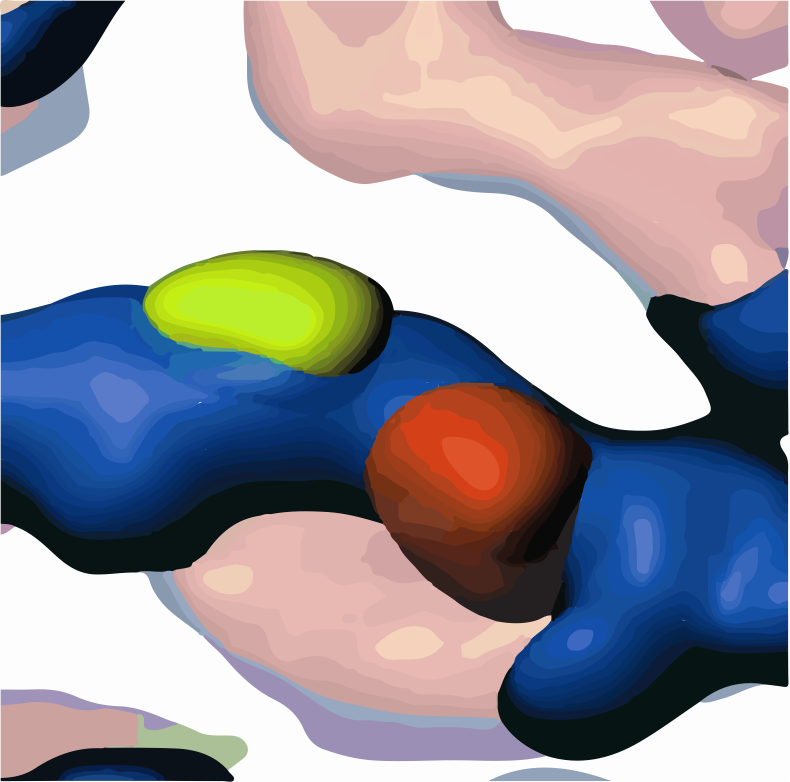
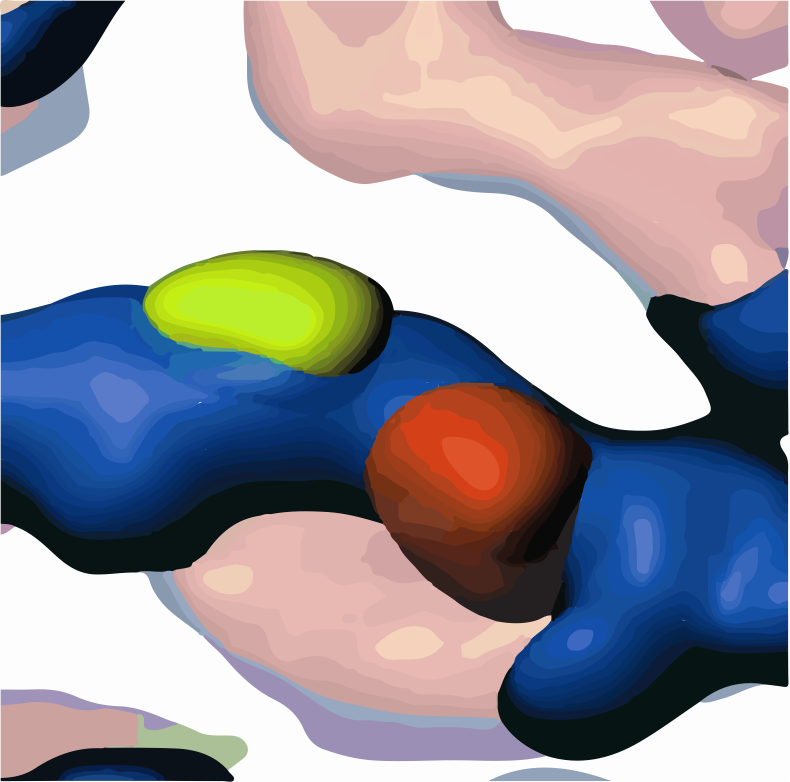
Confocal microscopy rendered image showing an HBV-specific GFP-CD4⁺ T cell (green), an HBV-specific DsRed-CD8⁺ T cell (red), and a Kupffer cell (blue) interacting in the liver of HBV-transgenic mice
Looking ahead
This study identifies a previously unrecognized, liver-specific immune circuit through which CD4⁺ T cells support antiviral CD8⁺ T cell function by activating Kupffer cells to produce IL-27. These findings broaden our understanding of tissue-specific immunity and suggest that IL-27 could be explored as a potential immunotherapy for chronic HBV.
“This work reveals a new axis of immune communication in the liver,” explains Dr. Valentina Venzin, first author of the study. “IL-27 was the unexpected link that brought everything together.”
“Importantly, this study challenges the traditional view that CD4–CD8 T cell interactions occur only in lymphoid organs,” adds Professor Iannacone. “We now provide a mechanistic description of such cooperation taking place directly in the liver. Future studies will be needed to determine whether this mechanism is also active in human disease.”
Written by: Laura Celotto
Published on: 30 June 2025
