News
World Hepatitis Day: expanding the treatment guidelines of hepatitis B
The World Health Organization estimated that in 2022 there were at least 254 million people worldwide suffering from chronic hepatitis B virus (HBV) infection.
This is likely an underestimate, as it is predicted that 87% of people living with HBV are unaware that they are infected as they have never received a diagnosis; this is especially true in low-middle income countries, where testing availability and vaccine coverage are scarce.
The underdiagnosis of HBV infection also leads to poorer treatment. In fact, it is calculated that only 3% of people with chronic hepatitis B (CHB) receive antiviral therapy globally.
Antiviral drugs consist of nucleoside and nucleotide analogues (NUCs) that block viral DNA elongation and help to keep chronic disease under control.
These orally available drugs, which are safe and well tolerated by most patients living with CHB, are nevertheless not prescribed to all of them, as shared international guidelines restrict their use to specific, eligible categories.
In a personal view piece published today in The Lancet Gastroenterology & Hepatology, key opinion leaders writing for the International Coalition to Eliminate HBV advocate for expanding the criteria to make anti-HBV drugs accessible to ALL CHB patients.
We spoke with Professor Luca Guidotti, Deputy Scientific Director at IRCCS San Raffaele Hospital, Full Professor of Pathology at Vita-Salute San Raffaele University, and a leading authority in the field - who is among the authors of the article and was honored in 2023 with the Distinguished Award in Hepatitis B Research, the most prestigious international accolade in the HBV field. We asked him why revising treatment guidelines for hepatitis B is now a critical priority.
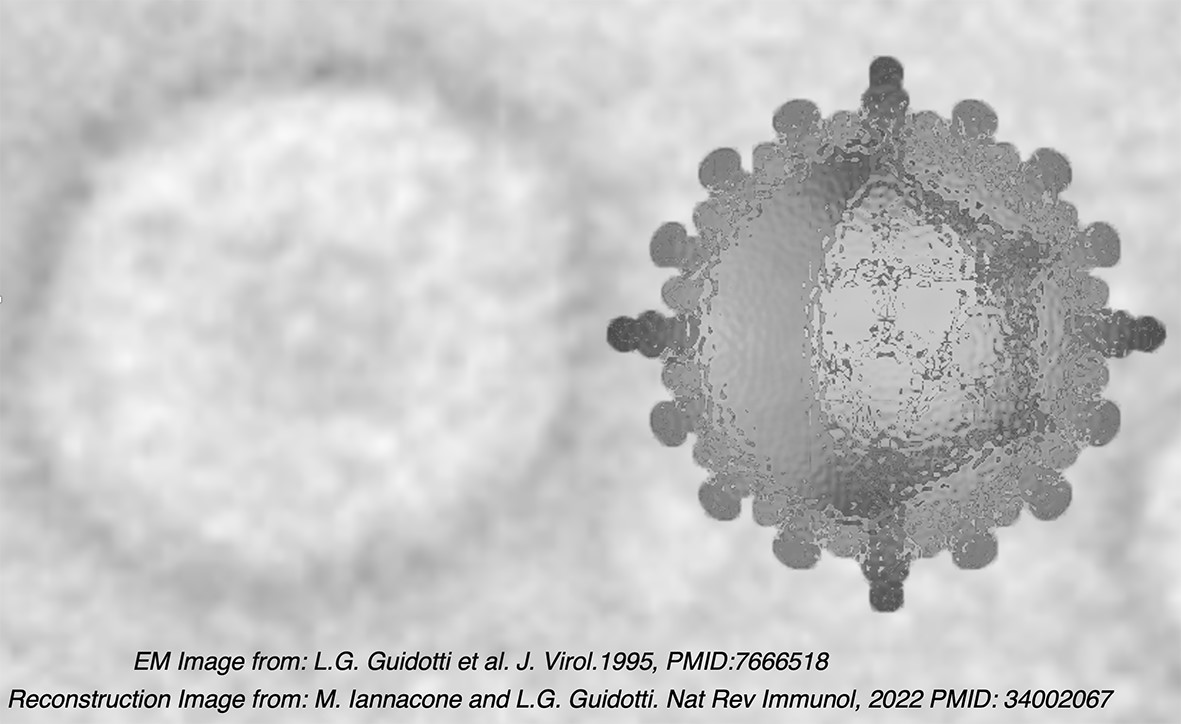
HBV is a sneaky virus
HBV mainly targets liver cells, called hepatocytes, but it is non-cytopathic per se, meaning that it does not kill infected cells. Thus, the virus replicates inside the hepatocytes without necessarily producing detectable signs or symptoms.
It is actually the host’s immune system that causes harm. When an infected person’s immune system recognizes viral antigens it kills the infected hepatocytes, thus triggering progressive inflammation and fibrosis of the liver, the characteristic symptoms of hepatitis B.
“The inflammatory liver environment, in turn, can dampen effective immune action, thus contributing to the persistence of the virus and possible chronicity of the infection,” explains Professor Guidotti.
In adults, HBV infection becomes chronic in up to 5% of the cases, but this percentage increases as the age of the infected person diminishes, reaching 90% or more in newborns if they are not vaccinated within their first months of life.
CHB patients require regular testing and ongoing monitoring to detect early signs of serious complications, such as liver fibrosis (scarring of the liver), cirrhosis (the advanced stage of fibrosis), or hepatocellular carcinoma (HCC), a primary form of liver cancer.
Fibrosis and cirrhosis primarily result from a sustained chronic inflammatory environment, which also favors mutagenesis at the basis of cancer development. HCC is also associated with possible integration of viral DNA within the cellular genome, which might produce unwanted mutations at the level of oncogenes or genes encoding for oncosuppressors.

Earlier and broader access to antiviral drugs might reduce the burden of hepatitis B and delay the onset of life-threatening complications
“Luckily, nowadays we can rely on NUCs to keep HBV replication under control and subsequently minimize the burden of disease chronicity.”, says Professor Guidotti.
As previously mentioned, NUCs inhibit the elongation phase of viral DNA synthesis, thereby suppressing HBV replication. This leads to reduced viraemia, limits viral spread, and lowers the likelihood of infecting new hepatocytes. Collectively, these effects help to mitigate liver inflammation, ultimately decreasing the risk of developing fibrosis, cirrhosis, and HCC. Additionally, the NUC-induced reduction in viral replication and viraemia is associated with decreased viral integration into the host genome, further contributing to a lower risk of HCC.
Current international guidelines restrict treatment with NUCs to people having more than 2000 IU/mL of viral DNA concentrations, liver enzymes (alanine aminotransferases) above the local upper limit of normal (ULN) or evidence of liver fibrosis.
“For this reason, in our personal view, we suggest revising and expanding such criteria, to aim for earlier and broader access to antiviral drugs.”, explains Professor Guidotti.
In this context, the authors suggest offering antiviral treatment to all people showing any detectable HBV DNA in the blood if any of the following criteria are met:
- Patients request treatment
- Patients have a family history of cirrhosis or hepatocellular carcinoma
- Patients are older than 30 years
- Patients have evidence of liver inflammation or liver damage
- People have comorbidities or risk factors that support treatment initiation
Among the potential drawbacks that could be associated with extended NUC therapy are:
- Kidney or bone pathology in up to 5% of treated patients
- Potential development of resistance to the virus against the drugs, due to incomplete viral removal
- Severe hepatic inflammation that could rebound upon drug withdrawal
- Expensiveness of treatment costs for patients living in some regions of the World
“We propose that the benefits of extending antiviral therapy outweigh the risks and might reduce the probability of developing cirrhosis or cancer”, says Professor Guidotti. “However, we also encourage the collection of extensive clinical data through further studies on the treatment of patients who fall outside the current guidelines to corroborate our proposals”, he concludes.
Published on: 28/07/2025
Author: Laura Celotto
